While the eyes may seem like simply organs of vision, they are far more than that—they can be indicators of underlying health conditions. In fact, certain systemic infections leave telltale signs in the eyes that can help clinicians diagnose diseases early. From viral to bacterial infections, the eyes offer a unique view into the body’s internal battles, sometimes revealing issues before they manifest elsewhere.
In this blog, we explore how different systemic infections can present through the eyes and why optometrists and ophthalmologists must be vigilant in recognizing these crucial signs.
Why Do Systemic Infections Show in the Eyes?
The eye is one of the most vascularized and immune-sensitive organs in the body, which makes it an ideal target for infections that spread through the bloodstream or nervous system. Viral, bacterial, and parasitic infections can all cause direct damage to ocular tissues or trigger immune responses that affect the eyes. This results in visible changes in the conjunctiva, retina, optic nerve, and other parts of the eye.
Ocular Signs of Common Systemic Infections
1. COVID-19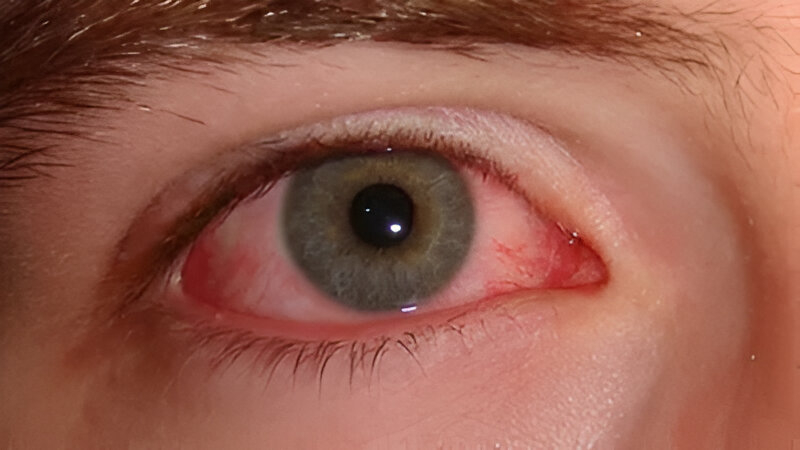
-
Ocular Manifestations: Conjunctivitis (pink eye), dry eye, irritation, and blurred vision.
-
Pathophysiology: The SARS-CoV-2 virus can enter the eye via the ACE2 receptor present in the ocular surface, potentially leading to viral conjunctivitis or dry eye symptoms.
-
Clinical Importance: Eye-related symptoms often appear in mild cases and may serve as an early warning sign, especially before the onset of respiratory symptoms.
2. Tuberculosis (TB)
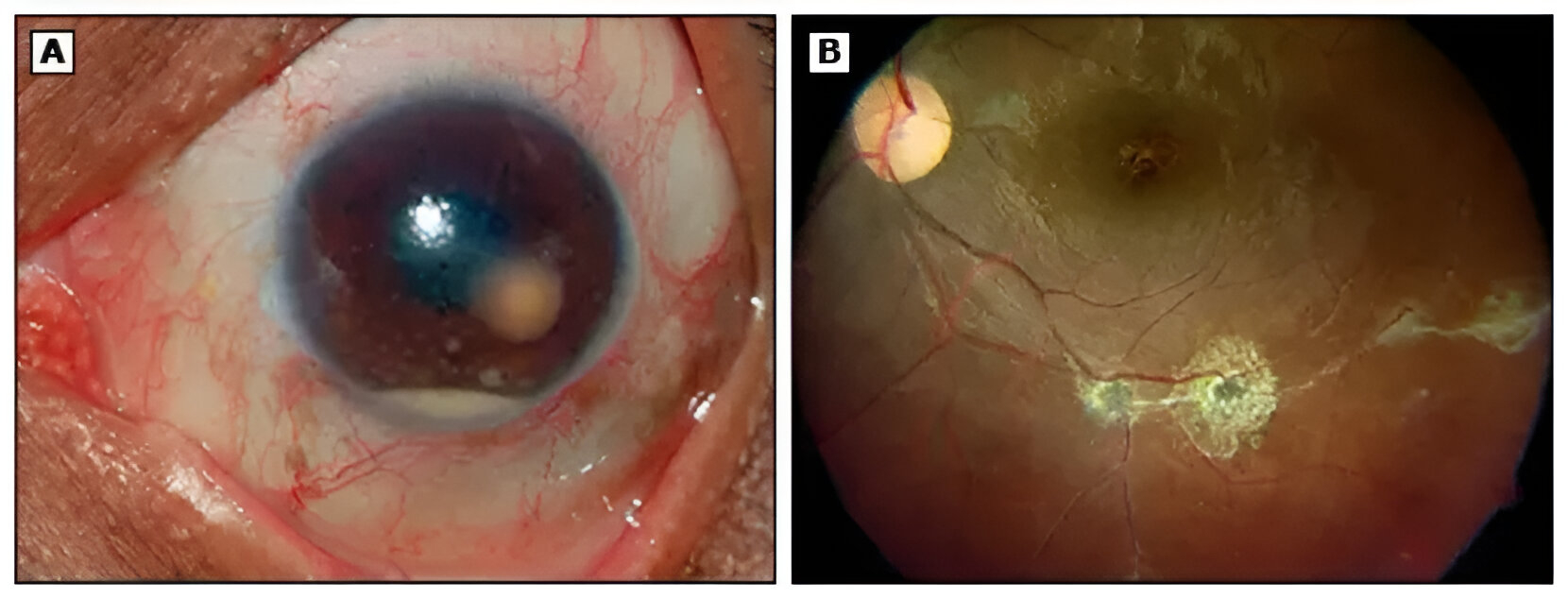
Anterior chamber granuloma due to ocular TB.
(A) Anterior chamber granuloma with granulomatous keratic precipitates and hypopyon.
Aspiration of the granuloma demonstrated acid fast bacilli in Ziehl-Neelsen stain.
(B) Following antituberculous treatment, the posterior segment demonstrates healed
pigmented scars along the vasculature. (©2014 UpToDate®)
-
Ocular Manifestations: Uveitis (inflammation of the uvea), choroiditis, optic neuritis, retinal vasculitis.
-
Cause: Mycobacterium tuberculosis can either directly infect the eye or trigger an immune-mediated response leading to inflammation.
-
Red Flag: Chronic or recurrent uveitis, especially in TB-endemic regions, should prompt further investigation for systemic tuberculosis.
3. HIV/AIDS
-
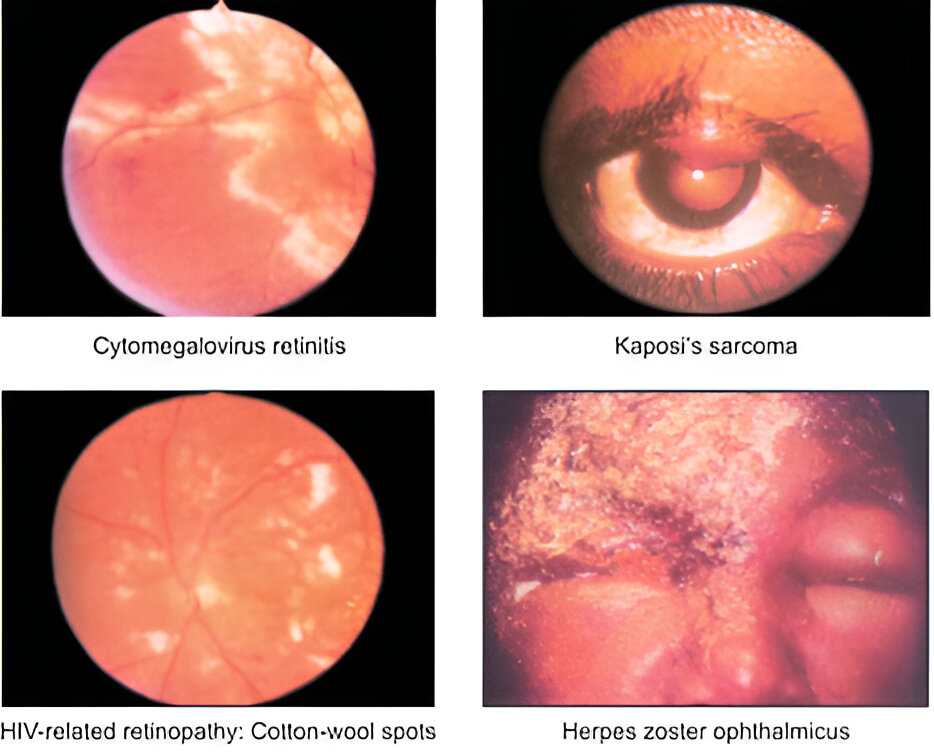
Ocular Manifestations: HIV retinopathy, cytomegalovirus (CMV) retinitis, Kaposi’s sarcoma of the eyelids, Herpes Zoster Ophthalmicus (HZO).
-
Opportunistic Infections: CMV retinitis, toxoplasmosis, and fungal infections can cause significant visual impairment.
-
Alert: New onset floaters or blurry vision in an HIV-positive patient warrants immediate referral to rule out these opportunistic infections.
4. Syphilis
-
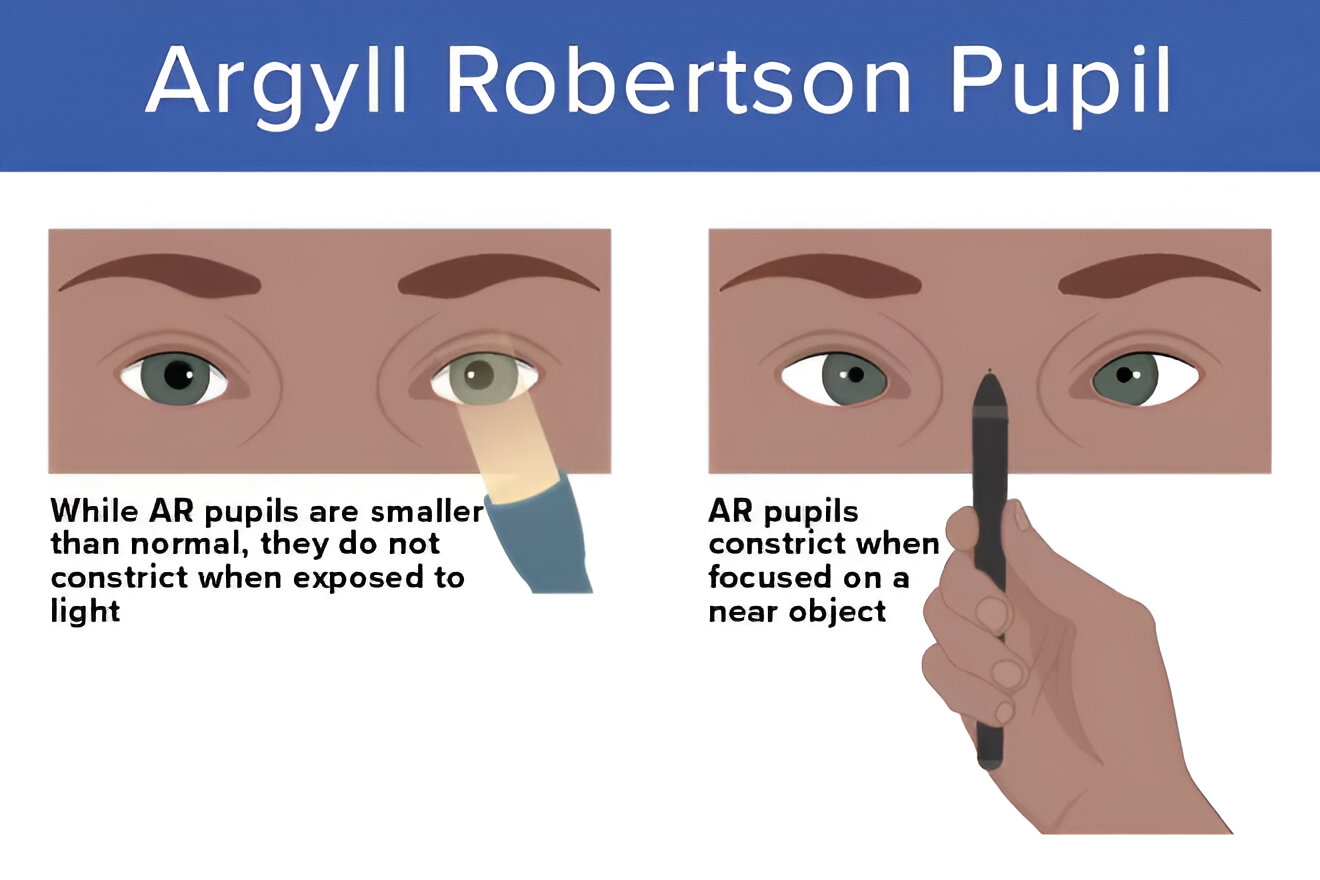
Ocular Manifestations: Uveitis, retinal vasculitis, optic neuritis, and the classic Argyll Robertson pupil (a constricted pupil that accommodates but doesn’t react to light).
-
Cause: The spirochete Treponema pallidum can affect the eye at any stage of the disease.
-
Diagnostic Tip: In cases of recurrent or unexplained uveitis, syphilis should be considered, especially in high-risk populations.
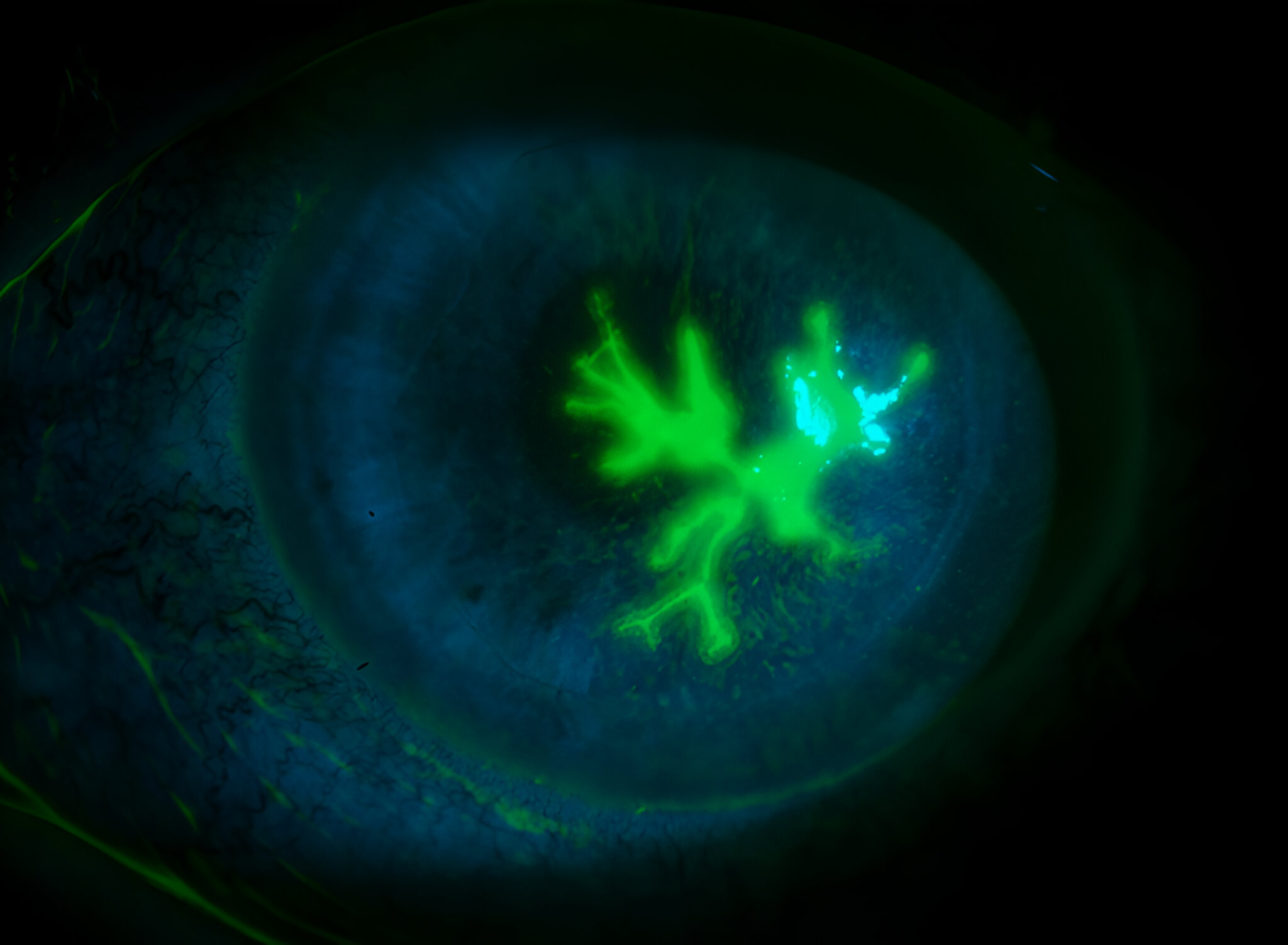
5. Herpes Simplex Virus (HSV) & Varicella-Zoster Virus (VZV)

-
Ocular Manifestations: Dendritic keratitis (HSV), stromal keratitis, and uveitis (VZV).
-
Special Consideration: Herpes Zoster Ophthalmicus (HZO) can lead to severe complications like corneal scarring, glaucoma, and vision loss.
-
Management: Early antiviral therapy is crucial for preventing long-term ocular damage from HSV or VZV infections.
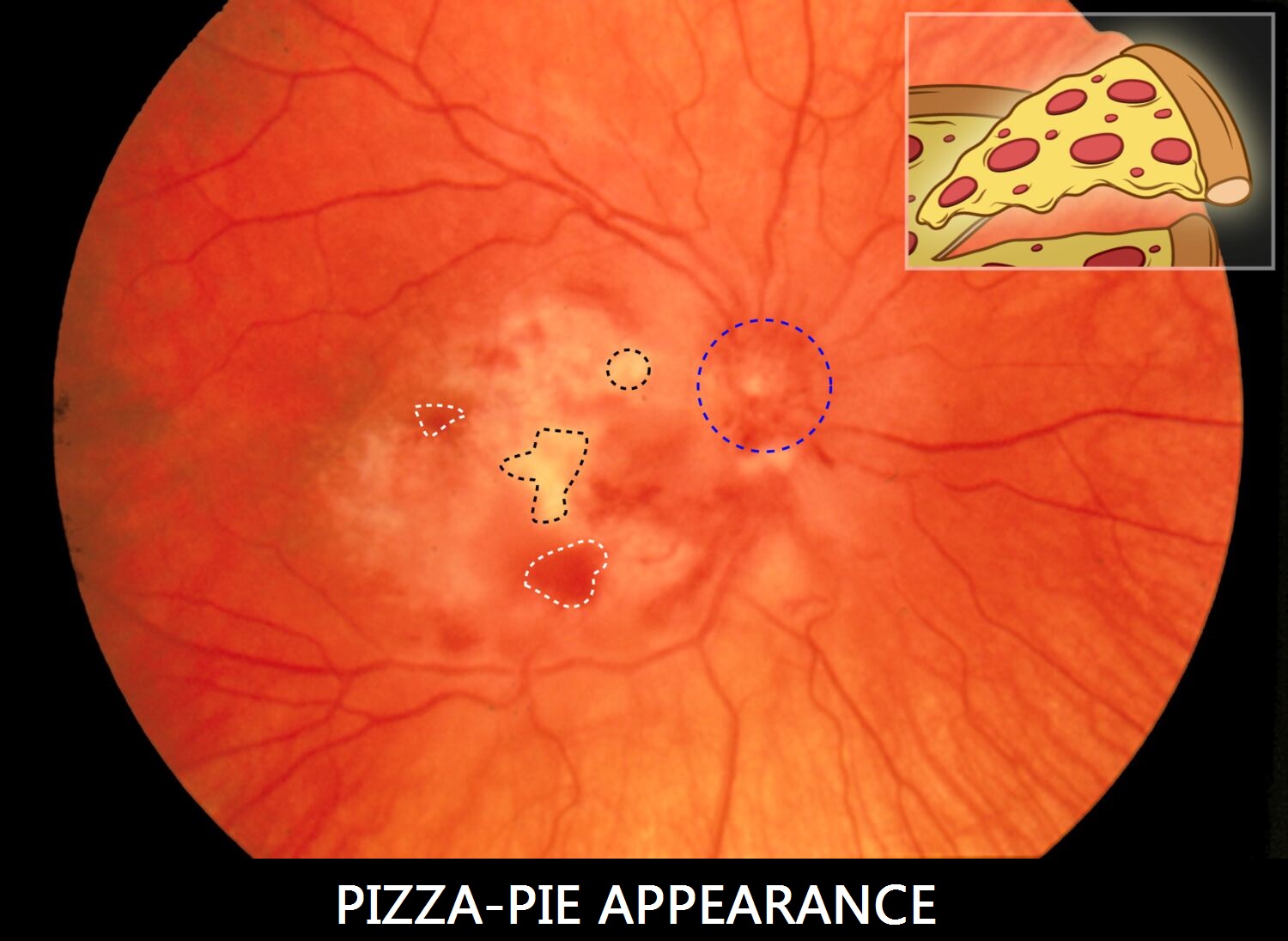
6. Cytomegalovirus (CMV) Retinitis
-
Manifestations: “Pizza pie” retinitis—a distinctive appearance with hemorrhages and retinal necrosis.
-
Associated with: Immunocompromised patients, particularly those with AIDS, organ transplant recipients, or those on immunosuppressive therapies.
-
Treatment: Systemic antiviral therapy (e.g., ganciclovir) is essential for managing CMV retinitis and preventing further vision loss.
7. Toxoplasmosis
-
Ocular Manifestations: Retinochoroiditis, often with a “headlight in the fog” appearance.
-
Cause: The parasitic infection caused by Toxoplasma gondii, typically acquired through undercooked meat or contact with infected cat feces.
-
Clinical Tip: Immunocompromised patients are at higher risk, and toxoplasmic retinochoroiditis is a leading cause of ocular inflammation in this population.
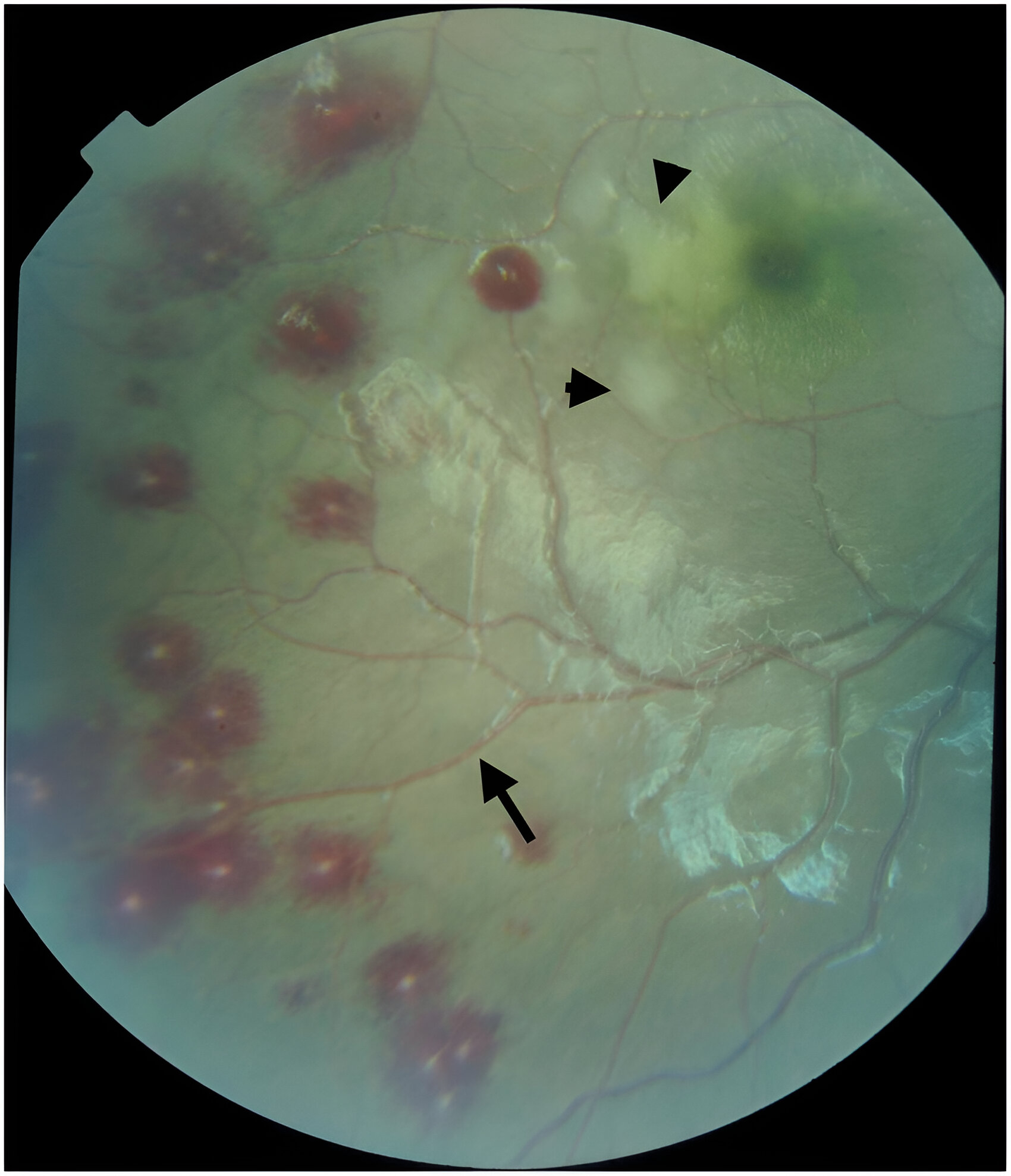
8. Malaria
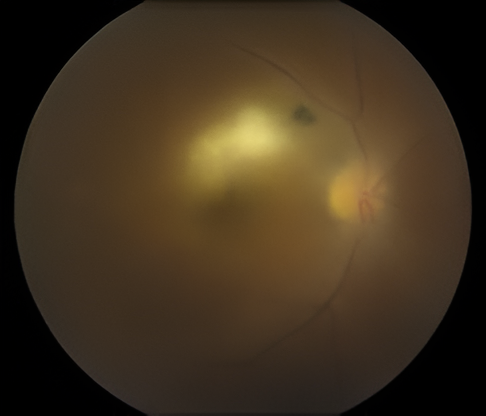
Malarial retinopathy: Retinal whitening, vessel changes, hemorrhages, and cotton wool spots etc.
-
Ocular Manifestations: Retinal hemorrhages, cotton wool spots, and in severe cases, retinitis or optic neuritis.
-
Cause: The malarial parasite (Plasmodium falciparum) can cause direct retinal damage due to vascular changes and inflammation.
-
Diagnostic Clue: Retinal findings should raise suspicion in patients with a history of recent travel to malaria-endemic regions.
Diagnosing Systemic Infections Through Ocular Signs
When systemic infections present with ocular manifestations, early diagnosis and intervention are crucial. Some common diagnostic tools to help in identifying these infections include:
-
Fundus Photography and Optical Coherence Tomography (OCT): These are used to examine retinal and macular changes, such as hemorrhages, edema, and choroidal inflammation.
-
Fluorescein Angiography: Helps visualize retinal blood flow and identify areas of leakage or ischemia.
-
PCR and Serology: Testing for specific pathogens (e.g., CMV, HIV, syphilis) through blood, vitreous samples, or even anterior chamber fluid.
-
Systemic Evaluation: Depending on the suspected infection, it may be necessary to conduct chest X-rays, blood cultures, or specific pathogen tests.
The Importance of Early Detection
Many systemic infections can be detected through the eye before they become severe. Timely identification of ocular manifestations can:
-
Prevent vision loss by initiating appropriate treatment early.
-
Improve overall prognosis for systemic infection through earlier systemic treatment.
-
Guide better patient management, as systemic infections often require multidisciplinary care involving infectious disease specialists.
Conclusion: The Eye’s Role in Diagnosing Systemic Infections
In clinical practice, a detailed eye exam can provide invaluable insight into a patient’s overall health. The eyes aren’t just for seeing—they’re also windows into the body’s systems, and recognizing the ocular signs of systemic infections can be life-saving.
As optometrists and ophthalmologists, we must remain vigilant and continue to educate ourselves about the latest findings in ocular manifestations of systemic infections. By doing so, we can ensure that we’re not just treating the eyes, but helping to protect the overall well-being of our patients.